The Thriving Illinois Kids Engagement Systematic (TIKES) Center
The Thriving Illinois Kids Engagement Systematic (TIKES) Center creates a unified education and research center focused on maximizing healthy developmental progress and social capital formation for the children in the state of Illinois. TIKES is the medical-home model that harnesses the power of information technology to identify and then deploy interventions to assist families and children at-risk for developmental social capital and thus future health and educational disparities. Building on existent cultural and family strengths, TIKES is longitudinal, developmentally focused, cost-effective and culturally relevant. TIKES focuses on digital health intervention development and population and chronic disease management and health costs. Since its inception in 2011, TIKES has undertaken more than $50 million in externally funded research.
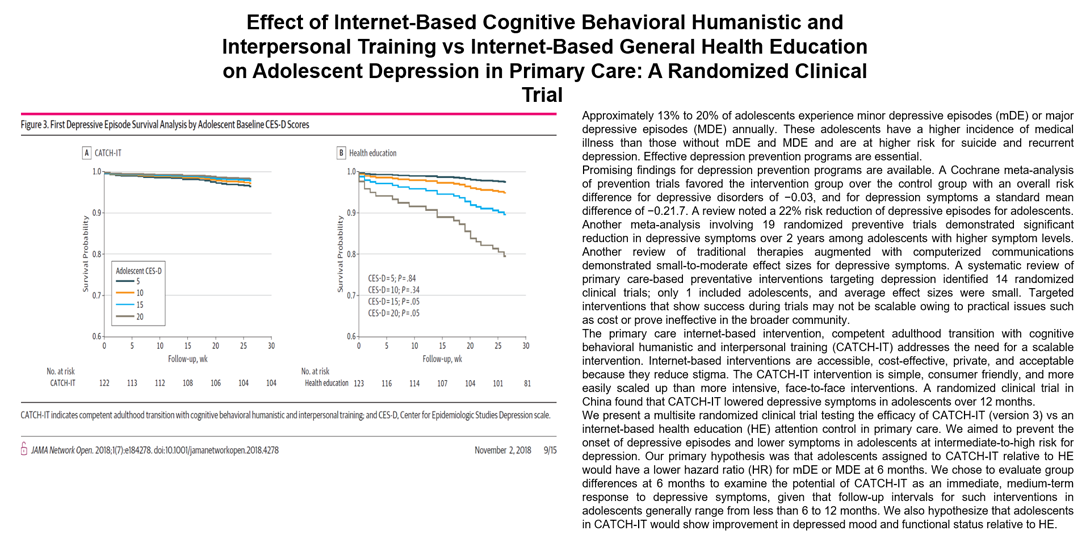
Digital Health Intervention (DHI) Development and population health: Dr. Benjamin W. Van Voorhees developed CATCH-IT (Competent Adulthood Transition with Cognitive, Humanistic, and Interpersonal Training), a primary care/internet-based adolescent-depression-prevention intervention in 2002 (N=14) and obtained funding (Centers for Disease Control) for and completed Phase 1 (Centers for Disease control, 2002-2004), Phase 2 multi-site dose/feasibility randomized clinical trials (K-08, NARSAD and RWJ Foundation support, N=83,2006-2011 ), Phase 3 (NIMH RO-1, N=369, 2011-2018) and phase 4 (PCORI, 2019-2027, NIMH, 2020-2025, PCORI 2022-2028). This intervention development has been supplemented by additional work, including the development of ethnically adapted versions of CATCH-IT: Chicago Urban Resiliency Building, (CURB, RWJ Foundation, 2010-2013), Chinese youth “Grasp the Opportunity” (Hong Kong Jockey Club, 2011-2014, phase 3 clinical trial completed), mainline China (trial under way), Arabic (clinical trial underway) and French versions (under development). HE also worked to develop peer-to-peer support and successfully conducted a randomized clinical trial (“Psychobabble”, adapted to primary care, NIMH R-34, 2007-2010, Vets Prevail, 2008-20011). Additional work has included implementation, epidemiology and case studies supporting the development of scalable depression-prevention models in health systema and community settings.
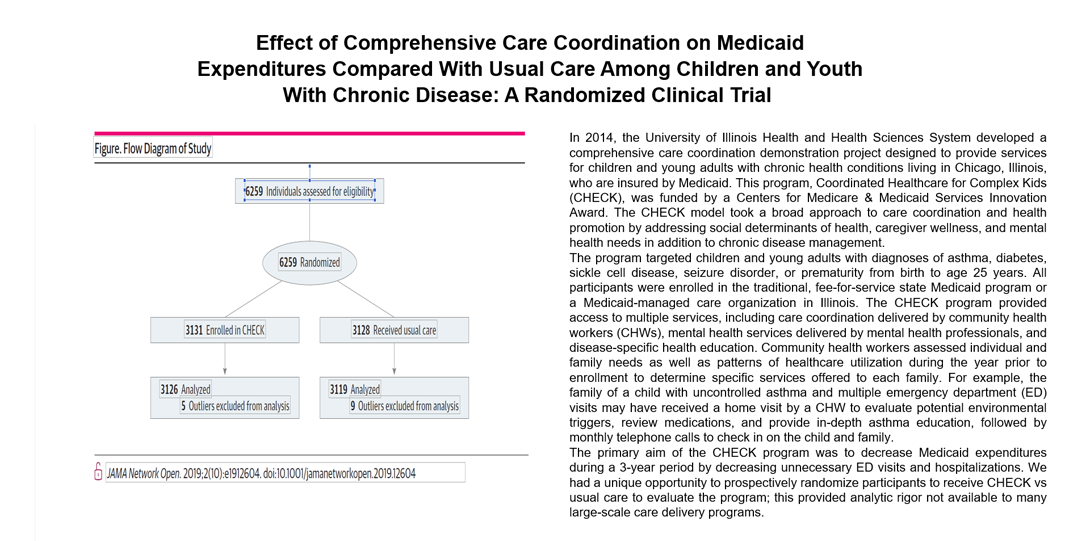
Chronic disease management and healthcare costs: September 2014, 1C1CMS331342-01-00 (Healthcare Innovation Award, Coordination of Healthcare for Complex Kids, $19,500,000, Benjamin Van Voorhees, Project Director). This project includes a multi-channel approach to reduce costs and improve outcomes in children and emerging adults with chronic diseases. The project eventually incorporated risk stratification and attempted to contact > 17,000 children, enrolled > 6,300 and provided > 230,000 services over four years using both technology and human contact.
Ongoing Research Projects Heading link
-
BEhavioral Health Stratified Treatment (B.E.S.T.) to Optimize Transition to Adulthood for Youth with IDD
B.E.S.T. is a Patient Centered Outcomes Research Institute-funded (AD-2020C3-21046), two-arm, randomized clinical trial seeking to examine the impact of care coordination models on the depressive and anxiety symptomology and transition outcomes of youth with intellectual and developmental disabilities (IDD). We want to understand if a care coordination model that includes integrated mental health programming is better at supporting youth with IDD in feeling healthier and happier than existing care coordination models that provide youth with IDD and referrals to outside mental health, as needed. B.E.S.T. seeks to recruit 780 youth with IDD, aged 13-20 years, who currently received care coordination services by 2026. As of May 2024, 269 youth with IDD have been enrolled in the study.
-
PATHway
PATHway is a NIMH-funded (1R01MH124723-01), multiphase-optimization-strategy (MOST) clinical trial seeking to optimize Competent Adulthood Transition with Cognitive Behavioral, Humanistic, and Interpersonal Training (CATCH-IT) for the prevention of depression in adolescents. While previous studies in the United States and China have been able to demonstrate effectiveness for CATCH-IT, we have encountered tolerability and scalability issues. We will use the MOST design to help prepare CATCH-IT for implementation studies and dissemination. We will be able to identify and eliminate non-contributing factors, while maintaining efficacy and strengthening tolerability and scalability. PATHway seeks to recruit 400 adolescents with mild-moderate symptoms of depressed mood, aged 13-18, by winter of 2024. As of October 2025, we have successfully concluded recruitment, with 400 adolescent participants enrolled.
-
PATH 2 Purpose
PATH 2 Purpose is a Patient Centered Outcomes Research Institute-funded (IHS-2017C3-9333), two-armed, comparative-effectiveness-randomized-control trial, evaluating the efficacy of two interventions: Teens Achieving Mastery over Stress (TEAMS) and Competent Adulthood Transition with Cognitive Behavioral, Humanistic, and Interpersonal Training (CATCH-IT). We are seeking to compare these two interventions early to prevent depressive illness and potentially other common mental health disorders. If effective, CATCH-IT would be able to provide a scalable, culturally acceptable, low-cost preventive intervention for mood disorders in adolescents, allowing health care providers to shift from a “wait until sick enough for treatment” model to a preventative model. PATH 2 Purpose seeks to recruit 634 adolescents who have mild-moderate symptoms of depressed mood in the 13-19 age range by summer of 2024. As of September 2025, have successfully concluded recruitment, with 636 adolescent participants enrolled.
Lab Members Heading link
Benjamin Van Voorhees
Benjamin Van Voorhees, MD, MPH
George R. Honig, MD, PhD, Endowed Professor in Pediatrics and Head, Department of Pediatrics
Professor of Medicine
Physician-in-Chief, Childrens Hospital University of Illinois
Department of Pediatrics, University of Illinois at Chicago
Children’s Hospital, University of Illinois Hospital & Health Sciences System
Email: bvanvoor@uic.edu
Tracy Gladstone
Tracy Gladstone, PhD
Associate Professor of Psychiatry and Human Behavior
Associate Professor of Behavioral and Social Sciences
Brown University
Email: tracy_gladstone@brown.edu
Calvin Rusiewski
Calvin Rusiewski, BMBS
Research Associate I
University of Illinois at Chicago
Email: crusiew2@uic.edu
Shion Kabasele
Shion Kabasele, Psy.M.
Research Associate II
University of Illinois at Chicago
Email: kabasele@uic.edu
Kristin Berg
Kristin Berg, PhD, AM
Associate Professor
University of Illinois at Chicago
Email: Kberg2@uic.edu
Iulia Mihaila
Iulia Mihaila, PhD
VST Research Assistant Professor
University of Illinois at Chicago
Email: milaila@uic.edu
Caterina Patriarca
Caterina Patriarca
Research Associate II
University of Illinois at Chicago
Email: cpatriar@uic.edu
Colleen Styles
Colleen Styles, PhD
Assistant Professor
University of Illinois at Chicago
Email: ecss@uic.edu
Kristen Kenan
Kristen Kenan, MD, MPH
Assistant Professor of Clinical Pediatrics
University of Illinois at Chicago
Email: kkenan@uic.edu
Osama Al Zoubi
Osama Al Zoubi, MD
Postdoctoral Research Fellow
University of Illinois at Chicago
Email: oalzou2@uic.edu
Brady Goodwin
Brady Goodwin, DO
Post-Doctoral Affiliate
University of Illinois at Chicago
Email: bradycgoodwin@gmail.com
Michael Gerges
Michael Gerges, MA, LCPC
Executive Director, CHECK
University of Illinois at Chicago
Email: mgergest@uic.edu
Helene Gussin
Hélène Gussin, PhD, MBA, MPH, CRA
Director of Administrative Operations
University of Illinois at Chicago
Email: hgussin@uic.edu
News Heading link
Grants Heading link
- #IHS-2017C3-9333 (Van Voorhees MD MPH: Co-PI)
Date: 03/01/2019-02/28/2024
Project: Primary Care and Community-based Prevention of Mental Disorders in Adolescents. - #IHS- 2017C3-9333 (Van Voorhees MD MPH: Co-PI)
Date: 7/15/2020-7/14/21
Project: Primary Care and Community Based Prevention of Mental Disorders in Adolescents - 1 R01 MH124723-01 (Van Voorhees MD MPH: Co-PI)
Date: 12/1/2020-10/31/2024
Project: Primary Care Based Depression Prevention in Adolescents: Intervention Optimization in Preparation for Implementation Study - #IHS- 106803 (Van Voorhees MD MPH: Co-PI)
Date: 112/1/2021-11/30/2027
Project: BEhavioral Health Stratified Treatment (BEST) to Optimize Transition to Adulthood for Youth with IDD - 3R01MH124723-04S1 (Van Voorhees: PI; Kenan: co-I)
Date: 1/10/2024-10/31/2024
Project: Diversity Supplement
Completed Projects Heading link
-
PATH Study, 2011-2018
Developing new interventions that incorporate the “diverse needs and circumstances of people with mental illness” – particularly in primary care and community settings – was a key NIMH strategic objective. Prevention of mental disorders had become a priority for the NIMH, which emphasizes the importance of developing “new and better interventions” to “…preempt the occurrence of disease.” These interventions were to (1) work in multiple and diverse settings (e.g. primary care); (2) be suitable for delivery outside of traditional mental health systems; (3) use new technologies; (4) build on previous clinical trials; (5) reduce identified disorders/enhance functional outcomes; (6) include families; and (7) be tailored to the individual. Despite these NIMH guidelines, while primary care physicians remain the first line providers for at-risk adolescents, there was no widely available, low-cost and culturally acceptable preventive approach that targets depression in primary care settings.
To address this gap and specified NIMH priority, Dr. Van Voorhees developed and conducted a phase 2 clinical trial of a primary care, Internet-based, depression-prevention intervention (CATCH-IT, Competent Adulthood Transition with Cognitive Behavioral Humanistic and Interpersonal Training). In this study, the high-intensity arm (i.e., motivational interview + internet site) demonstrated significant reductions in depressed mood and increases in protective factors (social support, motivation) and lower incidence of depressive episodes over 12 months (7% versus 28%), compared with the low intensity arm (internet site referral + only physician brief advice).
We now propose the next step study, a phase 3 efficacy study. In this 4-year, two-site randomized clinical trial, we propose to test the efficacy of the CATCH-IT primary care/Internet based depression prevention intervention against treatment as Active Monitoring Psych-education (AMPE) in preventing the onset of depressive episodes in an intermediate to high-risk group of adolescents aged 13-18. We plan to (a) identify high risk adolescents based on elevated scores on the PHQ-A, a screening measure of depressive symptoms; (b) recruit 400 (200 per site) of these at-risk adolescents to be randomized into either the CATCH-IT or the AMPE group; (c) assess outcomes at 2, 8, 12, 18, and 24 months post intake on measures of depressive symptoms, depressive diagnoses, other mental disorders, and on measures of role impairment in education, quality of life, attainment of educational milestones, and family functioning; and (d) conduct exploratory analyses to examine the effectiveness of this intervention program, moderators of protection, and potential ethnic and cultural differences in intervention response.
-
Coordinated Healthcare for Complex Kids (CHECK, 2014-2019)
CHECK was designed as a model that improves care for populations with specialized needs, with a focus on the specific priority area of high-cost pediatric and young adult populations. In addition, CHECK was designed to fit with a second Innovation category: models that test approaches for specific types of providers to transform their financial and clinical models (primarily pediatric providers who provide services to children with complex medical issues).
- Proposal goals: Our proposal aims were specified in the supplemental materials: 1) to reduce both inpatient admissions and emergency room visits, 2) to reduce missed school days and, 3) to increase patient satisfaction, activation, and engagement. By implementing early intervention approaches that focus on prevention of disease and preemption of exacerbations of chronic disease (Aim 1), we aimed to reduce hospital admissions and emergency room visits, garnering significant cost savings. CHECK’s cost savings were to pay for itself while also yielding savings for the Medicaid agency. Over and above these benefits, CHECK was to improve patients’ overall health, while also reducing missed school days and strengthening current and future productivity and quality of life (Aim 2). Aim 3 focused on building a population of satisfied, connected, engaged and activated patients who will experience greater health and well-being now and in the future, potentially reducing future healthcare costs.
- Target Population: Our target population was children and young adults with chronic health conditions. This was defined as patients under age 25 years who have either 1) a specific diagnosis of asthma, diabetes mellitus, sickle cell disease, or depression, or 2) two or more ongoing conditions from the following list: infectious diseases, diabetes mellitus, disorders of metabolism, sickle cell, splenic sequestration, depressive disorder, developmental delays, epilepsy, asthma, acute chest syndrome, intestinal malabsorption, other congenital anomalies of the heart, cleft palate, or perinatal disorders of the digestive system. The four specific targeted conditions were selected because of their prevalence in the population (including asthma, diabetes, and depression) or their complexity and cost (sickle cell), as well as the capacity and expertise within UI Health to address these conditions.
The 14 additional conditions were selected because internal data analysis had demonstrated that these were the most expensive disorders among this patient cohort (resulting from higher hospital admission and emergency room visit rates). We had expanded the age range to 25 years to include young adults with chronic diseases as this allows the case coordination to focus on improving the transition process for adolescents and young adults with special healthcare needs, a particularly disenfranchised population in Chicago (17% of young adult population). This transitional period proved critical in establishing patient utilization behaviors, and indeed effective healthcare during the transition to adulthood is essential for future health and productivity outcomes, including stable workforce participation, family formation, education, and peer relationships.
Please note that while this was our intended population, we were also fully open to engaging the Illinois Medicaid office to accommodate specific populations targeted by them as high-priority patients, if such changes had been conducive to care improvements from our program. (Of course, we would obtain proper approval from CMMI as well.)
- Number of beneficiaries served: We proposed to enroll 6,000 Cook County children and young adults in the CHECK program to have a real, measurable impact on pediatric health in our region.
- Number of participating providers: Including our FQHC partners, our network included about 250 total providers.
Service Delivery Heading link
Mental Health
- 8,800 mental health assessments
- 47,949 total mental health services
- 10,647 mental health consultations
- 7,055 direct mental health interventions
- 4,631 referrals
- 16,872 preventative interventions
Health Care Coordination
- 6,301 patients engaged in CHECK
- 183,525 total services delivered to patients
- 19,840 screenings and care plans
- 3,633 patient visits
- 15,470 successful contacts
- 27,331 health promotion/education services
- 17,221 referrals
- 8,294 consultations
Community Based Medical Neighborhood
- 14 clinical partners with 44 sites
- 42 dental mobile events serving 40 CHECK patients
Scholarship Heading link
- 26 manuscripts/articles in print, under review, or in progress
- 16 scientific presentations
Including, 2018 Pediatric Academic Societies, Scientific Session for Invited Science (Dr. Minier, Dr. Martin, Dr. Caskey, Dr. Pappalardo, Dr. Glassgow and Dr. Van Voorhees) - 10 grants submitted
Including, a U01 to the NIH-National Heart, Lung, and Blood Institute (Co-PIs, Dr. Martin and Dr. Caskey; Co-Is, Dr. Berbaum, Dr. Boucher-Berry, Dr. Glassgow, Dr. Hsu, Dr. Kim, Dr. Pappalardo, Dr. Pillers and Dr. Van Voorhees) - 20 faculty have contributed to CHECK scholarship
- Developed a nationally unique Database with more than 17,000 children and youth